Appendicitis is a sudden and often severe inflammation of the appendix that can escalate quickly if ignored. Recognizing the 4 stages of appendicitis helps patients and caregivers identify early warning signs, seek medical attention in time, and prevent potentially life-threatening complications. From mild discomfort and subtle digestive changes to severe rupture with high risk of infection, each stage has unique characteristics that require different levels of attention. Understanding these stages empowers people to act decisively, reduce emergency risks, and increase the chances of a safe recovery. The difference between catching appendicitis early and facing a medical crisis often comes down to knowledge and vigilance.
Introduction
Appendicitis is far more complex than a simple stomach ache—it is a progressive condition that moves through clearly defined stages, each carrying greater risk than the last. The 4 stages of appendicitis provide a framework for understanding how this common medical emergency develops and why timely intervention is so crucial. Early symptoms are often subtle, such as mild abdominal discomfort, nausea, or decreased appetite, which many people dismiss as minor digestive issues. Ignoring these warning signs can allow the inflammation to worsen rapidly, leading to complications such as rupture, peritonitis, or sepsis. By understanding each stage, patients can monitor their symptoms more accurately, recognize urgent red flags, and seek professional care before the condition escalates dangerously. Awareness and action at the right time are the keys to preventing serious outcomes.
Detailed
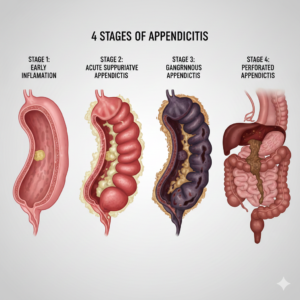
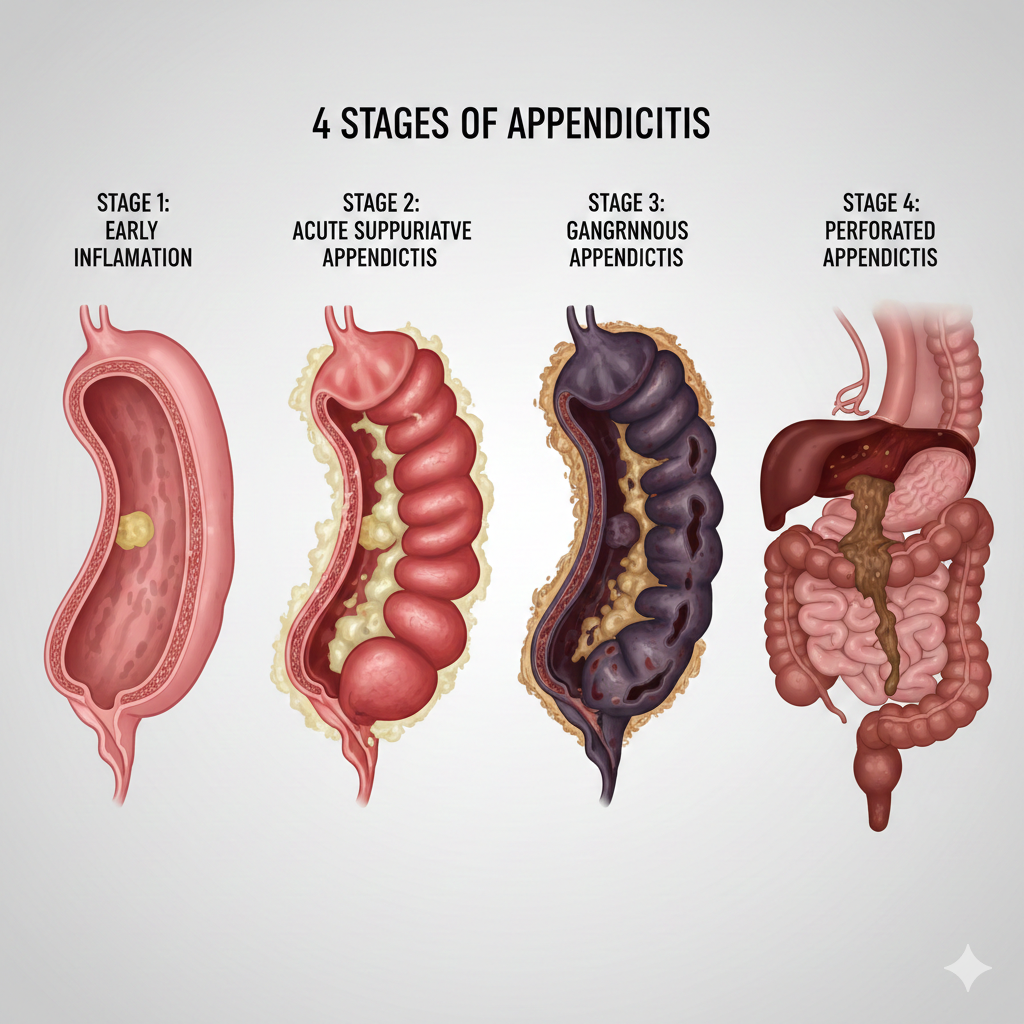
The appendix is a small, finger-shaped pouch attached to the large intestine, long considered a vestigial organ with no function. Modern research, however, suggests it plays a role in immune defense and gut flora balance. Appendicitis arises when the appendix becomes blocked, often by hardened stool, infections, or foreign objects, which leads to inflammation and swelling. Early in its development, symptoms can be very subtle: slight nausea, a vague ache near the navel, or a temporary loss of appetite. These early signs are frequently mistaken for indigestion or gas, delaying proper treatment. Understanding the onset of appendicitis is crucial because early detection allows intervention before the inflammation progresses to a more severe or life-threatening stage. Patients who act promptly often require less invasive surgery and have faster recovery times, while delayed action increases the likelihood of complications such as rupture, peritonitis, or prolonged hospitalization. Recognizing the warning signals of appendicitis is a vital step in safeguarding overall health.
Early Appendicitis (Mild Inflammation)
Stage 1 marks the beginning of appendicitis when the appendix’s inner lining becomes irritated and slightly swollen. Pain typically starts near the navel and gradually shifts to the lower right abdomen, often described as a dull or aching discomfort. Additional symptoms may include mild nausea, low-grade fever, and a temporary loss of appetite. The intermittent nature of pain and subtlety of symptoms often lead people to ignore them, making this stage particularly tricky to detect.
Medical professionals refer to this as the catarrhal stage. Inflammation is confined to the lining of the appendix, and no pus has yet accumulated. Early detection at this stage allows for timely surgical intervention, significantly reducing the risk of complications and ensuring a smoother recovery process.
Patients may notice discomfort worsening after meals, physical activity, or certain movements. Paying attention to persistent abdominal tenderness or changes in bowel habits can help catch appendicitis before it progresses to a more severe stage. Being proactive at this point can prevent the inflammation from advancing to acute appendicitis, which carries higher risks.
Ignoring these early signals can lead to disease progression. Understanding stage 1 symptoms is vital for early intervention, which not only reduces medical complexity but also alleviates anxiety by addressing the condition before it becomes urgent.
Pro Tips for Stage 1
- Observe subtle shifts in abdominal pain and its location over time.
- Avoid masking the pain with over-the-counter medications without medical guidance.
- Seek a medical consultation if mild discomfort persists or intensifies over 12–24 hours.
- Maintain a simple symptom diary to track changes in appetite, nausea, or bowel habits.
Acute Appendicitis (Increasing Inflammation)
Stage 2 occurs when the appendix inflames further, filling with pus and causing sharper, more persistent pain, usually concentrated in the lower right abdomen. The intensity of discomfort often increases during movement, coughing, or sneezing. Fever, nausea, and vomiting typically become more noticeable, while appetite continues to decrease. Pain may also radiate toward the back or hip, adding confusion for patients unfamiliar with appendicitis.
Known as the suppurative or phlegmonous stage, the appendix is at high risk of rupture if left untreated. Medical attention becomes urgent, as delays increase the likelihood of the inflammation spreading to surrounding abdominal tissue, leading to severe complications.
Other subtle signs may include constipation or diarrhea, abdominal bloating, and a noticeable sense of fatigue. Paying attention to these secondary symptoms, alongside the primary pain, can prompt earlier intervention. Early recognition significantly lowers the risk of progression to gangrenous appendicitis, which is far more dangerous.
Stage 2 emphasizes the need for timely medical consultation. Surgery or appropriate treatment at this stage is usually straightforward, but waiting too long can turn a manageable situation into a surgical emergency. Awareness and prompt action are crucial for optimal outcomes.
Pro Tips for Stage 2
- Keep detailed notes on symptom onset, duration, and severity to aid diagnosis.
- Avoid heavy meals to reduce digestive stress until medical evaluation.
- Monitor fever patterns and abdominal rigidity; escalating signs indicate urgent care.
- Maintain hydration but avoid large fluid intake before surgery evaluation.
- Also read this :Dentiloquent: Everything You Need to Know to Master Expressive Speech
Ruptured Appendicitis (Perforation)
Stage 3 is a critical turning point when the appendix tissue begins to die and perforates. The pain becomes severe, often spreading across the entire abdomen, and is accompanied by high fever, chills, nausea, and rapid heartbeat. This stage constitutes a life-threatening medical emergency.
Gangrenous appendicitis defines this stage. The risk of peritonitis—an infection of the abdominal lining—is extremely high. Immediate hospitalization and emergency surgery are essential to prevent sepsis and save the patient’s life.
Symptoms may include bloating, extreme tenderness, and overall weakness. Delays in seeking treatment at this stage can be fatal, highlighting the importance of recognizing and acting on earlier stage symptoms to prevent escalation.
Even after surgical removal of a ruptured appendix, recovery is often prolonged, with a higher risk of post-operative infections or complications. Awareness and education about the progression of appendicitis can prevent this stage altogether, making early recognition essential.
Pro Tips for Stage 3
- Call emergency services immediately if severe abdominal pain is accompanied by high fever or vomiting.
- Avoid self-medicating with antibiotics or painkillers without supervision.
- Post-surgery, follow all care instructions strictly to prevent infections.
- Ensure a support system is in place during recovery due to fatigue and weakness.
Chronic Appendicitis (Recurrent Episodes)
Stage 4 involves persistent or recurring inflammation of the appendix. Unlike acute appendicitis, pain is milder but lasts longer or appears intermittently. Digestive discomfort, mild nausea, or low-grade fever often accompany flare-ups. Chronic appendicitis is often overlooked because symptoms are subtle, yet repeated inflammation can cause scarring, blockages, or sudden acute episodes.
Chronic appendicitis may not require immediate emergency surgery, but monitoring is essential. Over time, recurrent inflammation can compromise digestive health and increase the risk of sudden progression to acute appendicitis.
Symptoms often resemble other digestive issues, such as irritable bowel syndrome or mild gastritis, making diagnosis tricky. Consulting a healthcare provider and performing diagnostic imaging can clarify the condition.
Patients experiencing recurring lower-right abdominal discomfort should never dismiss symptoms, even if mild. Preventative surgical removal may sometimes be recommended to avoid sudden emergencies, underscoring the importance of vigilance and professional guidance.
Pro Tips for Stage 4
- Keep a symptom diary to help doctors track flare-ups and duration.
- Schedule regular medical check-ups to monitor inflammation.
- Seek immediate care if mild chronic pain suddenly intensifies.
- Maintain a balanced diet and hydration to support digestive health.
Key Complications and Risks to Watch
Appendicitis carries significant risks if untreated. Rupture can lead to peritonitis, sepsis, or systemic infection, which can be fatal. Chronic inflammation may result in adhesions, blockages, or long-term digestive problems. Early detection and timely surgical intervention are the most reliable ways to prevent these serious complications, making patient awareness and vigilance critical at every stage.
Recognizing Red Flags
Red flags include sudden, severe lower-right abdominal pain, high fever, persistent vomiting, rapid heartbeat, and noticeable swelling. These signs require immediate medical attention, as they indicate advanced appendicitis or potential rupture. Early recognition of red flags can prevent life-threatening situations and improve surgical outcomes.
Summary of 4 Stages of Appendicitis
- Stage 1: Mild inflammation with subtle pain and nausea.
- Stage 2: Acute appendicitis with sharper pain, fever, and digestive symptoms.
- Stage 3: Ruptured appendix causing intense pain, fever, and risk of peritonitis.
- Stage 4: Chronic appendicitis with recurrent discomfort and potential for serious complications.
Understanding these stages equips patients to recognize early warning signs, reduce risks, and seek timely treatment, ultimately improving recovery and safety.
Conclusion: Don’t Wait—Act Fast
Appendicitis progresses rapidly, and each stage introduces greater risks. Knowledge of the 4 stages of appendicitis, awareness of early symptoms, and timely medical intervention can save lives. Early action reduces emergency surgeries, prevents severe infections, and ensures faster recovery. Listening to your body, recognizing warning signs, and seeking immediate care are the most effective ways to manage appendicitis safely.
FAQs
- What are the 4 stages of appendicitis?
The 4 stages are: Early (mild inflammation), Acute (increasing inflammation), Ruptured (perforation), and Chronic (recurrent episodes). - What are the first signs of appendicitis?
Early signs include dull pain near the navel, mild nausea, low appetite, and mild fever, often easy to overlook. - How can I tell if my appendicitis is severe?
Severe appendicitis often causes sharp lower-right abdominal pain, high fever, vomiting, bloating, and rapid heartbeat. - Is chronic appendicitis dangerous?
Yes, recurring inflammation can lead to blockages, scar tissue, or sudden acute attacks that require emergency surgery. - Can appendicitis rupture without warning?
Yes, if untreated, appendicitis can progress quickly, leading to rupture, peritonitis, or life-threatening infections. - When should I seek immediate medical attention?
Seek urgent care if you experience sudden severe pain, persistent vomiting, high fever, swelling, or rapid heartbeat. - Can appendicitis be prevented or detected early?
Early detection through awareness of symptoms, prompt medical evaluation, and preventive surgery in chronic cases reduces risks.
For more info :foxbreak.com